These days pills are available for abortion in all chemist shops for Abortion in Early Pregnanc...
Blogs by Dr. Anita Gupta, who is renowned as the best gynecologists for normal deliveries and caring during pregnancy.
Embracing Wellness: Your Guide to Women’s Health with Dr. Anita Gupta
- Published in Blogs by Dr. Anita Gupta
The Benefits of Natural Childbirth: What You Need to Know
Bringing a new life into the world is a remarkable journey filled with anticipation, joy, and sometimes, uncertainty. For many expectant parents, the concept of natural birth has gained significant traction in recent years, as they seek to embrace the beauty and empowerment of childbirth without medical interventions. But what exactly does natural birth entail, and what should you know before embarking on this path? Let’s delve into the essentials of natural birth.
Understanding Natural Birth
Natural birth, also known as unmedicated or physiological birth, is the process of delivering a baby without the use of medical interventions such as epidurals, induced labor, or cesarean sections, except in cases of medical necessity. Instead, it emphasizes the body’s innate ability to give birth and relies on techniques like breathing exercises, movement, and relaxation to manage pain and facilitate the birthing process.
The Benefits
Advocates of natural birth highlight several benefits:
- Empowerment: Natural birth allows expectant parents to actively participate in the birthing process, fostering a sense of empowerment and accomplishment.
- Faster Recovery: Without the use of medical interventions, recovery time may be quicker, enabling parents to bond with their newborn more swiftly.
- Reduced Intervention Risks: By avoiding medical interventions, potential risks associated with interventions, such as infections or adverse reactions to medication, are minimized.
- Bonding: The natural release of hormones during unmedicated childbirth, such as oxytocin and endorphins, can strengthen the bond between parents and their baby.
Preparation is Key
While natural birth can be a rewarding experience, adequate preparation is essential. Here are some key aspects to consider:
- Education: Educate yourself about the birthing process, including the stages of labor, breathing techniques, and coping strategies for managing pain. Attend childbirth education classes or workshops to gain valuable insights and skills.
- Support System: Surround yourself with a supportive birth team consisting of healthcare providers, doulas, and loved ones who respect your birth preferences and provide encouragement throughout the journey.
- Birth Plan: Develop a birth plan outlining your preferences for labor and delivery, including your stance on interventions, pain management techniques, and postpartum care preferences. Keep in mind that flexibility is crucial, as birth can be unpredictable.
- Physical Preparation: Engage in regular prenatal exercises such as yoga, walking, and pelvic floor exercises to strengthen your body and enhance flexibility, which can be beneficial during labor.
Coping Strategies During Labor
During labor, various coping strategies can help manage pain and promote relaxation:
- Breathing Techniques: Practice deep breathing exercises, focusing on slow, rhythmic breathing to promote relaxation and reduce tension.
- Movement: Experiment with different positions such as walking, swaying, or rocking to encourage optimal fetal positioning and alleviate discomfort.
- Massage and Counter pressure: Gentle massage and applying pressure to specific areas, such as the lower back or hips, can provide relief from contractions.
- Visualization and Affirmations: Use visualization techniques or repeat positive affirmations to maintain a positive mindset and channel inner strength during labor.
Embracing the Journey
Ultimately, the journey of natural birth is a deeply personal and transformative experience that varies for each individual. While it may come with its challenges, the sense of empowerment, connection, and joy that accompanies bringing a new life into the world can make it all worthwhile. By understanding the essentials of natural birth, adequately preparing, and embracing the support of your birth team, you can embark on this journey with confidence and grace, welcoming your little one into the world in the most natural and loving way possible.
- Published in Blogs by Dr. Anita Gupta
Planning a baby post 35 years of age
Planning a baby after 35 means first of all you may face difficulty in concieving naturally. There are two ovaries in a woman’s body close to the uterus. These form eggs which are fertilised with sperms to form pregnancy. With age the Ovarian reserve of eggs continues to decrease , especially after 35 years. Also post 35 the quality of your eggs may not be as good as at a younger age. Due to these reasons getting pregnant naturally may be difficult especially after 35 years of age.
Secondly post 35 the pregnancy may not be as smooth as at a younger age as incidence of genetic disorders like Down’s Syndrome is seen to increase with advancing age. We need to do special blood tests for this.
With advancing age there are more chances of getting high Bp or deranged blood sugars during pregnancy as compared to younger woman. So the pregnancy may fall into the high risk group requiring frequent and close monitoring. And sometimes premature delivery may also have to be done if these medical conditions get serious.
But there is no need to panic. If you plan pregnancy post 35 years it can be managed under the guidance of an expert and experienced Obstetrician.
- Published in Blogs by Dr. Anita Gupta
Laparoscopic Surgery
With technical advances these days there is trend of minimal invasive or Laparoscopic surgery performed for various gynaecological problems by a laparoscopic surgeon. A more advanced method is Robotic surgery performed by many laparoscopic surgeon in delhi and other bigger cities in India.
In these type of surgeries the cuts given are very small, usually less than one centimetre, so the post operative recovery is very good. Many times patient is discharged even on the same day. In these surgeries usually blood loss is also less. So where ever possible minimal invasive surgery done by a gynae laparoscopic surgeon is recommended.
- Published in Blogs by Dr. Anita Gupta
Safe Abortion tips and dealing with mental health of woman under going abortion
Abortion is a very common medical situation needing management under qualified medical personnel.
It is safe when carried out using a method appropriate to the pregnancy duration and under the guidance of a gynaecologist at a good medical centre.
Unsafe abortion can lead to maternal morbidity. It can lead to not only physical but also mental health problems.
Abortion may be done by choice when its an unplanned and unwanted pregnancy or it may be needed due to some medical problem in the pregnancy leading to missed or incomplete abortion.
Abortion can be performed using medication or a surgical procedure. In the first seven weeks of pregnancy, a medical abortion can be done using medicines. But it’s important to do it under proper guidance of a qualified gynaecologist after doing an ultrasound for pregnancy.
Post seven weeks usually a surgical method is performed which requires admission and the procedure in safer when done in an operation theatre under anaesthesia taking care of all aseptic measures and sometimes under ultrasound guidance.
If the abortion is done due to some medical issue or due to missed or incomplete miscarriage, it may lead to some mental issues, as it may have to be done suddenly as an emergency case. And in such cases the woman has the feeling of loosing her baby. They may have some depression for some but usually not requiring medication.
If the abortion is done by choice then usually it does not affect the mental status of the woman as she is well prepared for it.
By Dr. Anita Gupta
Associate Director
Obstetrics & Gynaecology
Fortis La Femme
- Published in Blogs by Dr. Anita Gupta
Contraceptive methods used to avoid getting pregnant
There are many methods for contraception but commonly used are Oral contraceptive pills, Intra uterine devices, Vaginal ring, Condom, Contraceptive injection, Contraceptive implant.
Oral contraceptive pills are of many types, all having hormones. Most effective are the combination pills with low dose hormones. The low dose ensures less side effects and the combination of hormones ensures regular menses and less chances of inter menstrual irregular bleeding or spotting per vaginum. These pills can be taken for many months/years. But it is better to start these after visiting a gynaecologist. One caution! Smoking and oral contraceptive pills is a very bad combination!!
The safer contraceptive with very very less failure rate are the various intra-uterine devices. There are two type of these devices; copper and hormonal. These have to be inserted in the uterus by a gynaecologist as a OPD procedure. Of these the hormonal ones are better, available by the name of Mirena which can be used for five years and then replaced with a new one. The copper devices are of two types which have to be replaced after every three or five years depending on the one used.
Then there are hormone loaded rings which are placed in the vagina every month and the lady can insert it on her own every time. This is also a safe contraceptive method with less failure rate. Only issue is using a new one every month.
Injectable contraceptives are also available with an efficacy of three months. This is also a very effective method but sometimes there is a side effect leading to irregular bleeding in those three months.
Very commonly used method is the barrier method where the male partner uses condoms. But this has the highest failure rate.
- Published in Blogs by Dr. Anita Gupta
Pregnancy care advice by the Gynecologist during Covid19
Pregnant woman fall in the category of higher risk when we talk of Covid 19. As During pregnancy you are more vulnerable to get infected with any disease as compared to a non pregnant woman because your immune system is comparatively more sensitive during pregnancy and post delivery. So pregnant ladies are considered to be in the high risk group just like aged people, children and also persons having co morbidity like diabetes or high BP, in this Covid pandemic.
So you need to be extra careful in this Covid-19 pandemic. So you need to take extra precautions. Take care of yourself by maintaining proper social distancing and good hand hygiene. Cover your nose and mouth properly with a mask when stepping out. In fact avoid unnecessary movements outside your home. Eat healthy food. Have lot of fruits and vegetables. Keep yourself well hydrated by taking plenty of water and other liquids like nimbu pani and coconut water. Try to do small walks inside your house. Keep your rooms well ventilated.
 Avoid going out unnecessarily. Try to get most of the things home delivered. Use a mask when receiving your groceries and other stuff. If you are visiting the Gynecologist or Hospital for your routine checkup then wear the Mask properly and maintain social distancing. Carry your own water bottle and a small snack. Before taking an appointment for a physical checkup ask your Gynecologist for Online consultation if it can be done.
Avoid going out unnecessarily. Try to get most of the things home delivered. Use a mask when receiving your groceries and other stuff. If you are visiting the Gynecologist or Hospital for your routine checkup then wear the Mask properly and maintain social distancing. Carry your own water bottle and a small snack. Before taking an appointment for a physical checkup ask your Gynecologist for Online consultation if it can be done.
Tele consultation is usually possible in the first four months of pregnancy. Try to avoid unnecessary hospital visits.
Continue taking all your vitamins, iron, calcium and protein supplements. Follow all your doctors instructions. If any doubt do tele consultation. Be aware of baby movements. Report to hospital if you experience any fever, lethargy or muscle pains. Don’t be afraid if you are told to get yourself tested for Covid.
Live healthy. Eat healthy. Sleep healthy. God forbid if inspite of all precautions you still get Covid positive, then follow Gynecologist’s instructions carefully. Many pregnant women have recovered and have had healthy babies.
Author: Dr. Anita Gupta, Gynecologist in Delhi
- Published in Blogs by Dr. Anita Gupta
Ovarian Cysts: Symptoms and Causes
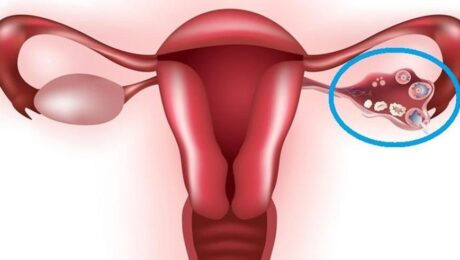
The ovaries are a very important part of a female body. They (Ovarian Cysts) are in a pair in the female reproductive system and are located one on each side of the uterus. Each ovary is about the size and shape of an almond. The ovaries produce eggs and are also the main source of the female hormones estrogen and progesterone. They influence the development of a woman’s breasts, body shape, and body hair. They also regulate the menstrual cycle and pregnancy.
Ovarian Cysts Symptoms
A cyst is a fluid-filled sac and can be located anywhere in the body. Ovarian cysts are fluid-filled sacs or pockets within or on the surface of an ovary. Different types of cysts can form in the ovary. Many cysts are completely normal. These are called functional cysts and these are very commonly found. They occur during egg formation. Functional cysts normally shrink over time, usually in a few months.
When to Know That You Fall in High Risk Pregnancy Group
If you have a functional cyst, you may need a check-up once again in 1 to 2 months to make sure that the cyst has become smaller or has completely resolved. These cysts are almost never associated with cancer. But if you are menopausal and are not having periods, you will not have functional cysts.
The other types of cysts are chocolate cysts, Simple cysts, or dermoid cysts. Many women have ovarian cysts without having any symptoms it is advisable to meet a gynecologist in Delhi. In some the cyst will cause these problems:
- Pressure, fullness, or pain in the abdomen
- Pain during sexual intercourse
- Painful menstrual periods and abnormal bleeding
- Nausea or vomiting
To identify the type of cyst, the following tests are needed:
- Pelvic ultrasound
- CA 125 blood test- It is a tumor marker and is often elevated in ovarian cancer.
The ovarian cysts can be treated in the following ways:-
- Wait and watch: The patient waits and gets re-examined in one to three months to see if the cyst has changed in size. This is a common treatment option for women who are in their childbearing years, have no symptoms, and have a simple cyst less than 5 cm size.
- Surgery: If the cyst does not go away after few menstrual cycles, has become larger, or looks unusual on the ultrasound, causes pain, or the woman is postmenopausal, then there is a need to remove it.
There are two surgical methods:
- Laparoscopy- if the cyst looks non-cancerous on the ultrasound, CA-125 is normal then laparoscopy can be done. This procedure is done under general anesthesia. Very small incisions of 0.5 to 1.0 cm are needed in this surgery.
- Open Surgery- if the cyst is solid and looks suspicious, then open surgery is needed. The incision in open surgery is sometimes quite big.
- Published in Blogs by Dr. Anita Gupta
Early Signs of Pregnancy
This type of situation is not very common
Early Signs of Pregnancy Symptoms
Pick Your Right Gynecologist / Obstetrician in South Delhi
- Published in Blogs by Dr. Anita Gupta
When to Know That You Fall in High Risk Pregnancy Group
If you miss your menses date by more than a week, the first thing to check should be pregnancy, do a home test. You get many types of pregnancy checking kits in chemist shops. Buy one and check with the first urine early morning. If positive see a Gynecologist (obstetrician in Delhi) at the earliest.
If your age is more than 35 years (which is quite common these days as women are now career-oriented) then you are a candidate whose pregnancy falls into the high-risk pregnancy group as with advancing age there are more chances of problems for the mother and the baby both. Similarly, if you have got your pregnancy after treatment for infertility or through IVF (test tube baby) then also you come into this group.
Follow the advice of your Gynaecologist sincerely and carefully. Go for regular check-ups. Do all the tests asked for as in these pregnancies some extra tests are needed most of the time. Take all the prescribed medicines regularly
- Published in Blogs by Dr. Anita Gupta